Heat Safety & Performance Coalition Resources
HSPC provides resources that are tailored to employers, supervisors, and workers to assist with effective implementation of occupational heat safety. Implementing heat safety best practices will optimize worker health, safety and productivity. Learn more about why heat safety practices should be implemented, how your organization can do it, and who is more susceptible to heat-related illnesses and injuries!

Employer Resources
How can employers implement a heat plan to protect your employees? How can heat safety initiatives make workers more productive? Why are heat safety plans so important? These resources can be used by employers and provide materials such as heat safety onboarding information, a “how to guide” for implementation of heat safety plans, emergency action plan templates, and more to create a safe workplace.
New Employee Onboarding
If applicable, new employees should complete a physical examination prior to heat exposure to identify pre-existing medical conditions that are associated with heat intolerance. Physical exams must be conducted in compliance with HIPAA and federal regulations regarding employee protection.
During Onboarding, employers should inform employees of the following:
- Risk factors associated with heat-related illness
- Signs and symptoms of heat-related illness
- Strategies to mitigate heat-related illness (heat acclimatization, hydration, body cooling,etc)
- Locations of hydration and rest stations
- Details of the heat safety plan
- The appropriate chain of communication that must occur during an emergency
Emergency Action Plan
What is an Emergency Action Plan and why is it important?
Emergency Action Plans (EAPs) contain vital information on policies and procedures that should be taken during a potentially catastrophic event. While emergencies are rarely predictable, they do occur and the response that occurs in the first 5-10 minutes will likely dictate the outcome. Everyone involved (supervisors, workers, security, etc.) be educated on, have access to and rehearse the EAP. Rehearsal should occur at least annually, but the more frequent the rehearsals, the more efficient the response when an emergency arises.
Once an EAP is established, it is imperative that it is implemented effectively via posted copies/distribution, education on the EAP for all personnel, and routine rehearsals of the EAP.
What can I do to prepare for an emergency?
- Make sure your employer and supervisor have gone over the EAP with you and you have a clear understanding of your role if an emergency was to arise.
- Ask questions and know how to get in contact with your supervisor for an emergency.
- Review the EAP at least annually.
What is my role?
In most instances, workers are going to the best first people to respond to an emergency. It is important to be able to recognize the signs and symptoms associated with heat illness and cardiac emergencies. You should know who the first aid responder is on your shift and the best way to get a hold of them if an emergency. If you are the first person to respond to an emergency, you should know where the nearest phone is to call 911 and then move individual inside or to a shaded place and remove excess clothing.
Get help. Send someone to find the supervisor or give them a call from your phone.
Heat Safety Plan
1. Commit to a heat safety plan
Safety must come FIRST. Your organization’s commitment to a heat safety plan represents a dedication to keeping your workers safe from the dangers of heat. By going the extra mile and caring for your employee/worker's health, well-being, and safety, your organization will develop a strong reputation. Committing to a heat safety plan can also reap financial rewards through heat safety training and reducing productivity losses associated with heat stress (Decreased worker's compensation, decreased time out of work, etc).
If your organization has multiple worksites, it may require multiple heat safety plans (e.g., large corporations, power plants).
2. Designate a heat safety officer for your company and identify specific roles for management team
Once your organization is committed, they will need to designate roles and make sure management is on board. Ask the following questions:
- Who will be creating and reviewing heat safety plans?
- Who is supervising workers to ensure they are following the plan?
- Who will train the employees?
- Who will assess the effectiveness of the heat safety plan after implementation?
Creating a safety committee to discuss the implementation of the heat safety plan is important to ensure that the heat safety plan is feasible. Involving the workers with the heat safety committee will aide in determining feasibility while encouraging them to follow the plan once it is in place.
3. Examine your organization’s current adoption of heat safety practices
Examine what policies your worksite already has in place to protect workers from heat exposure. Safety officers and employers should ask themselves the following questions:
- Do we have a specific written heat safety plan in place?
- If so, what are its components? Are the current guidelines evidence-based?
- If not, does the organization already instill safety practices that could also protect workers from heat stress
Be prepared to create or alter your heat safety plan based on what you found while reviewing your current policies. Your heat safety practices should be made to follow the current standard guidelines and be evidence-based to best protect your workers from heat illness.
4. Assess worksite safety hazards
To optimize heat safety, you must identify what heat hazards currently exist in your organization. For example, are workers performing work around radiant sources of heat, such as ovens? Safety officers should:
- Inspect all job sites for hazards.
- Review surveillance data for accidents, injuries, etc related to heat.
- Get feedback from your workers. What heat hazards do they feel impact their health and productivity?
5. Create your heat safety plan!
Now that you’ve: 1) committed to heat safety, 2) created a team, and 3) assessed current policies/procedures and workplace hazards associated with heat, it's time to create the plan!
Utilizing the recommendations created in the published occupational heat safety document (pending publication) will help guide employers and safety managers with the creation of a heat safety plan.
Organizations should reach out to heat safety experts at NHSC to review the plan prior to implementation.
6. Gather heat safety resources, training material, and supplies
Once your organization has created a heat safety plan, the resources, training materials, and supplies will need to be collected or created. Utilize the resources on this site or others such as OSHA or NIOSH to translate the heat safety plan to your workers.
Training materials should be created for the onboarding process and annual heat safety training. Once a new plan is implemented, supervisors should be trained to ensure they understand the new standards for surveillance and safety purposes. Once workers are trained, all employees (workers and supervisors) must confirm their readiness to implement the plan. Workers should know exactly what to do and when they need to do it. No plan is perfect, so supervisors should be prepared for surveillance and feedback following the implementation of the heat safety policies.
7. Continuing education: always update your plan!
As new research comes out on heat safety, more occupational heat safety recommendations will be offered. It's important to continuously educate yourself and others on new developments in the world of heat safety and revise your heat safety plan accordingly.
Cost To Benefit
Implementing Occupational Heat Safety Practices Save Money!
Cost of Productivity Loss Due to Heat
Absenteeism: Worker Compensation Claims
Examples from OSHA fatalities for exertional heat stroke>
New York
At 3:30 p.m. on August 2, 2018, an employee was working at a recycling plant and was shredding plastic. Employee was working at recycling plant and presented at the emergency room personnel with signs of heat stroke.
Violation Cost: $20,329
https://www.osha.gov/pls/imis/establishment.inspection_detail?id=1336350.015
Nebraska
At 11:15 a.m. on July 13, 2018, an employee was working at a farm in the fields. During work, the employee became overheated and began to get disoriented. The employee strayed away from the other workers, suffered a heat stroke, and died. When the supervisor realized that the employee was missing, a search party was organized. The employee was found dead the next morning. The autopsy report attributed the cause of death to heat stroke.
Violation Cost: $11,641
Florida
At 2:00 p.m. on August 25, 2018, an employee was using a lawn edger for approximately 6 hours and began to feel lightheaded. The employee was placed in the shade and given a sports beverage and water to drink. The employee began to feel better and went back to work where he soon passed out and was unresponsive. The employee began to have "seizure-like" activity and experienced multiple organ failure, severe dehydration, and hyperthermia. The employee is killed.
Violation Cost: $16,102
Presenteeism: Reduced Physical Work
Examples from:
- Morabito M, Messeri A, Crisci A, et al. Heat-related productivity loss: benefits derived by working in the shade or work-time shifting. Int J Product Perform Manag 2020;70:507–25. doi:10.1108/IJPPM-10-2019-0500
- Foster J, Smallcombe J, Hodder S, et al. An advanced empirical model for quantifying the impact of heat and climate change on human physical work capacity. Int J Biometeorol 2021;:1–15. doi:10.1007/s00484-021-02105-0Economic Cost = Worker’s Salary x Productivity Loss (%) (1)Productivity Loss is a loss in physical capacity to do work, which affects work output
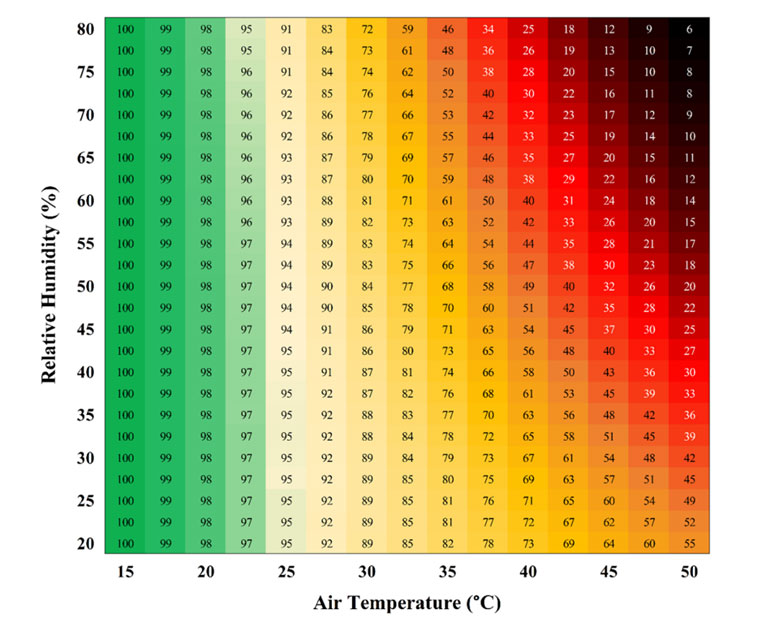
Physical capacity losses based on air temperature and Relative Humidity (2).
Example:
Worker Daily Salary: $400 per day
Ambient Temperature: 35° C
Relatvie Humidity: 45%
Economic Cost for one employer undergoing heat stress
Economic Cost = $400 x 0.71 = $284
The organization will have lost $284 dollars per worker per day based on the environmental conditions and worker daily salary.
10 workers = $2,840 a day!
100 workers = $28,400 a day!
Cost of Heat Safety Plan
Example: Cooling Vests
One cooling vest = approximately $50 per worker
10 workers = $500
100 workers = $5,000
For 100 workers: will you invest $5,000 for cooling equipment to save $28,400 a day
Supervisor Resources
HSPC provides resources tailored to supervisors who are in charge of supervising the implementation of heat safety plans and best practices. These resources can be used to learn more about dangers of heat and assist supervisors with implementation of heat safety practices.
Workers at risk of Heat Illness
As a supervisor, you must be aware of workers who are at greater risk of developing a heat-related injury or illness. Workers who have the following conditions are at an increased risk for heat illness:
Non-Modifiable
- Type 1 Diabetes
- Heart Disease
- Autonomic Dysfunction
- Hyper- and Hypo-hidrosis
- Kidney Pathology
- Medications that affect thermoregulation, central nervous system function and sodium balance
Modifiable
- Sedentary Lifestyle
- Type 2 Diabetes
- Obesity
If you have workers with any of these conditions, the following precautions should be taken prior to occupational exposure in a hot environment:
- Identification of the pre-existing condition through medical monitoring
- Pre-placement evaluation
- Fit-for-duty evaluation
The following education and preparation should be encourage for the worker:
- Proper hydration
- Adequate sleep
- Increased fitness levels
- Notifying a supervisor of recent illness
Epidemology
Fatality rate = 0.22 per million workers
359 occupational heat-related deaths were identified between 2000 and 2010, which corresponds to a fatality rate of 0.22 per 1 million workers. Gubernot et al. (2014) Heat-exposed agricultural workers were 14% more likely to experience a traumatic injury compared to non-heat exposed agricultural workers. Spector et al. (2019)
Problem? 13.3 MILLION workers perform work in heat per day!
Help us keep workers safe from heat-related illnesses and injury!
Cardiac Emergency Procedures
Men
- Chest pain, angina and / or neck pain
- Severe headache
- Excessive breathlessness
- Vague malaise
- Dizziness / palpitation
- Increasing fatigue
- Indigestion / Heartburn / Gastrointestinal symptoms
Women
- Center chest pain - comes and goes
- Lightheadedness
- Shortness of breath with/without chest discomfort
- Uncomfortable pressure/squeezing/fullness
- Nausea/vomiting
- Cold Sweat
- Pain/discomfort in one or both arms, back, jaw, neck, and/or stomach
How to identify cardiac arrest
Responsive
Monitor vitals: pulse rate/quality, breathing rate/quality, blood pressure, skin temp/color, pupils
Health History
S– Signs/symptoms
A– Allergies
M– Medications
P– Past health information
L– Last intake
E– Events leading up
Unresponsive
Assess Airway, Breathing, Circulation (ABC’s)
Pace maker and medical alert bracelet
Ask questions to bystanders
Emergency Procedure
- Send someone to get Supervisor and activate EMS
- Be prepared to answer questions about what happened when EMS arrives
- If trained in CPR and AED - be prepared to assist in CPR
Workers Resources
Workers undergoing heat stress must understand how heat can negatively affect their health, safety and productivity. These resources are tailored to the worker and provide educational materials for workers who are characterized as “at-risk”, temperature monitoring, heat illness emergency procedures, and more to keep them safe on the job.
At Risk of Heat Illness
Who is at an increased risk of Heat Illness?
- Individuals living a sedentary lifestyle
- Type 1 and Type 2 Diabetes
- Heart Disease
- Obesity
- Hypertension (high blood pressure)
- Autonomic Dysfunction
- Hyper-hidrosis (excessive sweating)
- Hypo-hydrosis (decreased sweating)
- Kidney Pathology
- If you are taking medications that could affect thermoregulation Central nervous system function and/or sodium balance
I have one of the above conditions. What should I do next?
- Inform a supervisor
- Ensure proper daily hydration
- Get a good night's sleep
Emergency Action Plan
Emergency Action Plans (EAPs) contain vital information on policies and procedures that should be taken during a potentially catastrophic event. While emergencies are rarely predictable, they do occur and the response that occurs in the first 5-10 minutes will likely dictate the outcome. Everyone involved (supervisors, workers, security, etc.) be educated on, have access to and rehearse the EAP. Rehearsal should occur at least annually, but the more frequent the rehearsals, the more efficient the response when an emergency arises.
Once an EAP is established, it is imperative that it is implemented effectively via posted copies/distribution, education on the EAP for all personnel, and routine rehearsals of the EAP.
What can I do to prepare for an emergency?
- Make sure your employer and supervisor have gone over the EAP with you and you have a clear understanding of your role if an emergency was to arise.
- Ask questions and know how to get in contact with your supervisor for an emergency.
- Review the EAP at least annually.
What is my role?
In most instances, workers are going to the best first people to respond to an emergency. It is important to be able to recognize the signs and symptoms associated with heat illness and cardiac emergencies. You should know who the first aid responder is on your shift and the best way to get a hold of them if an emergency. If you are the first person to respond to an emergency, you should know where the nearest phone is to call 911 and then move individual inside or to a shaded place and remove excess clothing.
Get help. Send someone to find the supervisor or give them a call from your phone.
Heat Exhaustion vs Heat Stroke
Heat Exhaustion
- Core temp < 105°F
- Irritability
- Fainting
- Decreased muscle coordination
- Dizziness/Light-headedness
- Headache
- Chills
- Nausea or vomiting
- Diarrhea
- Decreased blood pressure
- Pale
- Fatigue
- Heavy Sweating
- Weakness
- Decreased Urine Output/Dehydration
- Hyperventilation
Heat Stroke
- Core Temp > 105°F
- Irritability, irrational behavior, emotional instability
- Altered consciousness
- Disoriented/confused
- Dizziness
- Headache
- Looks "out of it"
- Nausea or vomiting
- Diarrhea
- Muscle cramps, loss of muscle function/balance, inability to walk
- Collapse or staggering
- Feeling sluggish
- Profuse sweating (or dry skin?)
- Decreasing performance or weakness
- Dehydration, dry mouth, thirst
- Rapid pulse, low blood pressure, quick breathing
Emergency Procedures
- Move the individual to a cool/shaded area and remove excess clothing
- Elevate legs to promote venous return
- Call for supervisor or send someone to get supervisor
- Assist with cooling the individual with fans, rotating ice towels, or ice bags
- Provide oral fluids for rehydration
Heat Stroke
- Remove excess clothing and equipment
- Call supervisor or send someone to get supervisor
- Assist in cooling the individual as quickly as possible (whole body ice water immersion is the gold standard). This should be done within 30 minutes. Help by continuously stirring water and adding ice throughout the cooling process.
- If immersion is not possible, take individual to shaded, cool area and use rotation cold, wet towels to cover as much of the body surface as possible
- Help to maintain airway, breathing and circulation
Cardiac Emergency Procedures
Men
- Chest pain, angina and / or neck pain
- Severe headache
- Excessive breathlessness
- Vague malaise
- Dizziness / palpitation
- Increasing fatigue
- Indigestion / Heartburn / Gastrointestinal symptoms
Women
- Center chest pain - comes and goes
- Lightheadedness
- Shortness of breath with/without chest discomfort
- Uncomfortable pressure/squeezing/fullness
- Nausea/vomiting
- Cold Sweat
- Pain/discomfort in one or both arms, back, jaw, neck, and/or stomach
How to identify cardiac arrest
Responsive
Monitor vitals: pulse rate/quality, breathing rate/quality, blood pressure, skin temp/color, pupils
Health History
S– Signs/symptoms
A– Allergies
M– Medications
P– Past health information
L– Last intake
E– Events leading up
Unresponsive
Assess Airway, Breathing, Circulation (ABC’s)
Pace maker and medical alert bracelet
Ask questions to bystanders
Emergency Procedure
- Send someone to get Supervisor and activate EMS
- Be prepared to answer questions about what happened when EMS arrives
- If trained in CPR and AED - be prepared to assist in CPR